Medication Kidney Warning Checker
This tool helps you recognize potential signs of medication-induced kidney inflammation. It is not a diagnosis tool and does not replace professional medical advice. If you experience any symptoms, consult your healthcare provider immediately.
Check Your Symptoms
Select any symptoms you're experiencing that might relate to kidney inflammation:
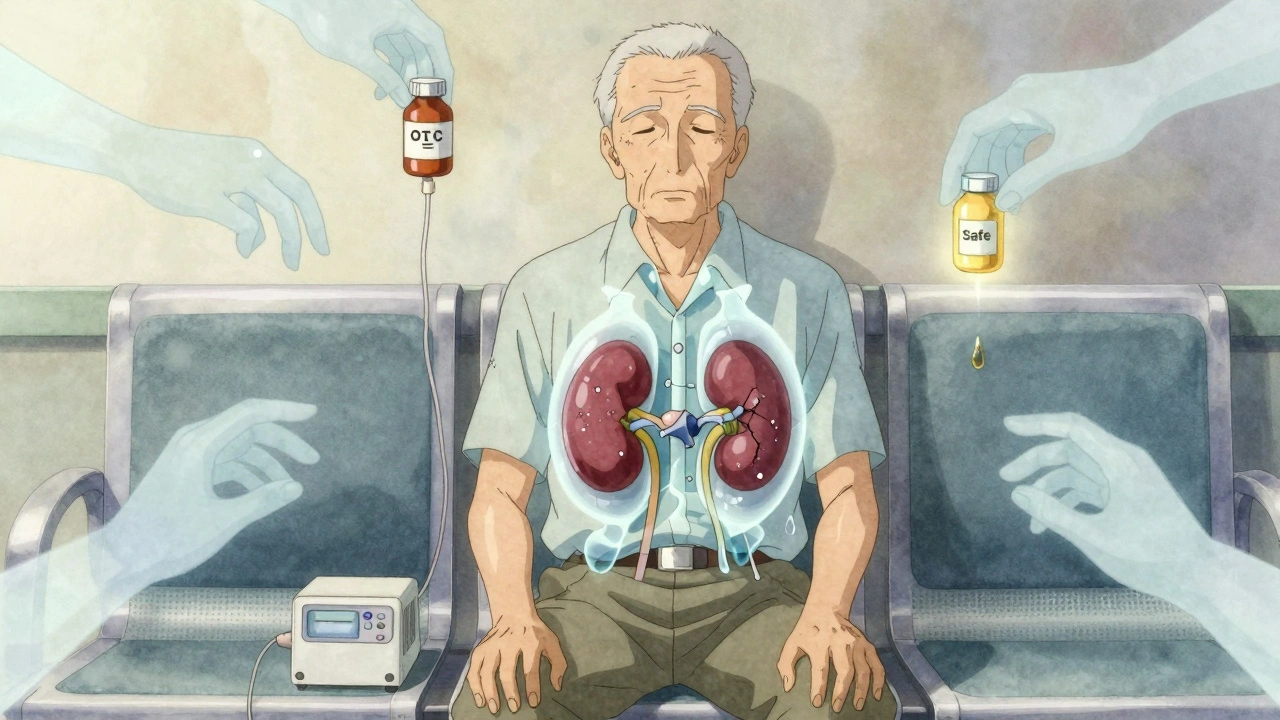
Most people don’t think about their kidneys until something goes wrong. But when a common medication triggers acute interstitial nephritis, the damage can happen fast - and often goes unnoticed until it’s serious. This isn’t rare. Every year, thousands of people develop kidney inflammation because of drugs they took for heartburn, pain, or infection. And the scary part? Many doctors miss it.
What Exactly Is Acute Interstitial Nephritis?
Acute interstitial nephritis (AIN) is inflammation in the spaces between the kidney’s tubules. These tiny areas help filter waste and balance fluids. When they swell, the kidneys can’t work right. The result? A sudden drop in kidney function, often called acute kidney injury (AKI).
Unlike infections or dehydration, AIN from medications is an immune reaction. Your body sees a drug as a threat and sends immune cells into the kidney tissue. It’s not an allergy like a rash from penicillin - it’s deeper, quieter, and harder to spot.
The most common triggers? Antibiotics, proton pump inhibitors (PPIs) like omeprazole, and NSAIDs like ibuprofen. Over 250 drugs have been linked to AIN. The FDA started requiring warning labels on PPIs in 2021 because of how often they cause this reaction.
Signs You Might Have Medication-Induced Kidney Inflammation
There’s no single symptom that screams “AIN.” That’s why it’s so often mistaken for a urinary tract infection, dehydration, or just aging.
- Less urine output - You’re not peeing as much as usual. This happens in about half of cases.
- Fever - Not always high, but persistent. Often comes with no other signs of infection.
- Rash - Not always red or itchy. Sometimes just a faint pink patch.
- Swelling - Ankles, legs, or face puff up because the kidneys can’t flush out fluid.
- Fatigue and nausea - Feeling wiped out or sick to your stomach without explanation.
Here’s what’s misleading: The classic “hypersensitivity triad” - fever, rash, and eosinophilia (high white blood cells) - only shows up in fewer than 10% of cases. So if you don’t have all three, it doesn’t mean you’re safe.
What really matters are lab results. A rise in serum creatinine by 0.3 mg/dL in 48 hours or 1.5 times your baseline within a week is a red flag. And if you’ve been on a new medication in the past 3 months? That’s a huge clue.
Which Medications Are Most Likely to Cause This?
Not all drugs carry the same risk. Some are common culprits - and you might not even realize they’re dangerous to your kidneys.
- Antibiotics - Beta-lactams like ampicillin and methicillin cause 35-40% of cases. Fluoroquinolones like ciprofloxacin are also high-risk. Symptoms usually appear 1-2 weeks after starting the drug.
- Proton pump inhibitors (PPIs) - Omeprazole, pantoprazole, esomeprazole. These are taken daily for heartburn, often for months. AIN from PPIs shows up later - usually 10-12 weeks after starting. Despite milder symptoms, recovery is slower than with antibiotics.
- NSAIDs - Ibuprofen, naproxen, diclofenac. People take these for arthritis or back pain, sometimes for years. AIN from NSAIDs often comes with heavy protein in the urine - over 3 grams a day - which is unusual for other types of AIN.
- Immune checkpoint inhibitors - Used in cancer treatment. These are newer triggers, but they’re rising fast. They cause bilateral kidney involvement and often need long-term steroid treatment.
What’s surprising? Over-the-counter drugs are just as dangerous as prescriptions. A 2022 study found that 40% of patients didn’t tell their doctor they were taking ibuprofen or PPIs daily. They thought it was harmless.

How Is It Diagnosed?
There’s no blood test that confirms AIN. That’s why kidney biopsy is the gold standard.
Doctors start with a urinalysis. Look for:
- Sterile pyuria - White blood cells in urine, but no bacteria. Happens in 70-90% of cases.
- Eosinophiluria - Eosinophils (a type of immune cell) in urine. Found in 30-70% of cases. This is a strong hint, but not everyone has it.
- Mild proteinuria - Usually under 2 grams per day. But NSAID cases can spike above 3 grams.
If these signs are there and you’ve been on a suspect drug, a biopsy is next. It shows immune cells swelling the kidney tissue, inflamed tubules, and sometimes eosinophils. The best time to do it? Within 3-7 days of symptoms starting. Wait too long, and scarring sets in.
New tools are emerging. A blood test for neutrophil gelatinase-associated lipocalin (NGAL) can detect early kidney stress with 85% accuracy. But it’s not widely available yet.
What Happens If It’s Not Treated?
Early action saves kidneys. Stop the drug, and many people recover fully - especially if they’re under 50.
But delay? That’s where things go wrong.
- 15-25% of untreated cases turn into chronic kidney disease.
- Up to 10% end up needing dialysis.
- Older adults and those on multiple medications have the worst outcomes.
One patient on a forum shared: “I took omeprazole for 3 months. My kidneys dropped to 30% function. Stopping the drug helped, but I’m still at 75% after 8 weeks of steroids.” That’s not rare.
Another case: A 68-year-old man took ibuprofen daily for arthritis. He didn’t feel sick until he couldn’t pee. It took 4 months to recover - and he still has high blood pressure from kidney damage.
How Is It Treated?
Step one: Stop the drug. Immediately. Don’t wait for test results. If you suspect AIN, stop the medication within 48 hours.
Step two: See a nephrologist. Within 24-48 hours. They’ll check your kidney function, order imaging, and decide if a biopsy is needed.
Step three: Steroids? That’s where opinions split.
The European Renal Association recommends steroids if kidney function doesn’t improve after 7 days of stopping the drug. The American Society of Nephrology says only use them if creatinine is above 3.0 mg/dL.
Why the disagreement? No randomized trials prove steroids work. But observational studies show faster recovery when they’re used. In practice, about half of nephrologists prescribe them.
If steroids are used, it’s usually prednisone at 0.5-1 mg/kg per day, tapered over 4-6 weeks. Side effects? Weight gain, mood swings, high blood sugar. But for someone with failing kidneys, the risk of not treating is worse.
Who’s Most at Risk?
This isn’t random. Certain people are far more likely to develop AIN:
- People over 65 - They make up 65% of cases, even though they’re only 16% of the population.
- Those on five or more medications - Polypharmacy increases risk 4.7 times.
- Women - 1.8 times more likely than men to develop drug-induced AIN.
- People with existing kidney issues - Even mild CKD makes you more vulnerable.
And here’s the kicker: PPI use among adults over 65 is projected to rise from 38% in 2020 to 45% by 2030. That means more AIN cases - unless doctors start asking better questions.
What Should You Do?
If you’re on any of these drugs - antibiotics, PPIs, NSAIDs - and you notice any of these changes:
- Less urine
- Swelling in legs or face
- Fever with no cold or flu
- Unexplained fatigue or nausea
Don’t wait. Talk to your doctor. Say: “Could this be kidney inflammation from my meds?”
Keep a list of everything you take - including supplements and OTC drugs. Many patients don’t mention ibuprofen or antacids because they think they’re “safe.” They’re not.
And if your doctor dismisses your concerns? Push for a basic kidney panel: serum creatinine and urine analysis. If those are abnormal, insist on a nephrology consult.
AIN is preventable. It’s treatable. But only if you catch it early.
What’s Next for AIN Research?
Science is moving fast. A 2023 study found a genetic marker - HLA-DRB1*03:01 - that makes people 4.2 times more likely to develop AIN from PPIs. In the future, genetic testing could warn high-risk patients before they even start these drugs.
AI tools are being trained to predict AIN from electronic health records. One algorithm spotted patterns in medication use and lab trends with 89% accuracy.
And a major NIH trial (INTERSTIC) is testing new immunomodulators that might replace steroids - with fewer side effects.
But for now, the best tool is awareness. Know the signs. Know your meds. Ask the question before it’s too late.

Lucinda Bresnehan
December 2, 2025 AT 16:27I took omeprazole for years thinking it was harmless. My creatinine jumped last year and I didn’t even connect it until my nephrologist asked if I was on acid reflux meds. I cried. I had no symptoms except feeling tired all the time. Please, if you’re on PPIs, get a simple blood test. It’s not dramatic, but it’s life-changing.
Shannon Gabrielle
December 3, 2025 AT 12:35Oh great another ‘meds are secretly killing you’ post. Next you’ll tell me water is a silent assassin. I’ve been on ibuprofen since 2010 and my kidneys are fine. Your fearmongering is why people don’t trust doctors anymore.
ANN JACOBS
December 3, 2025 AT 22:06It’s truly remarkable how modern medicine has become so reliant on pharmaceutical interventions that we’ve forgotten the body’s innate capacity to heal - and how easily we overlook the subtle, systemic consequences of chronic drug exposure. The kidneys, those quiet, tireless filters, are not invincible. Their decline is often silent, and the cultural normalization of daily NSAIDs and PPIs is a public health quiet crisis. We must shift from reactive to preventative paradigms - not just for kidneys, but for our entire physiological ecosystem.
Kshitij Shah
December 3, 2025 AT 23:42Bro in India we take 3 ibuprofen before breakfast and call it a day. My uncle had kidney issues and he blamed it on chai. Not the meds. Everyone’s just lucky here. Or dumb. Maybe both.
Bee Floyd
December 5, 2025 AT 02:33I didn’t know this was a thing until my mom got diagnosed. She’s 71, on 7 meds, and thought her fatigue was just ‘getting old.’ Turns out it was PPIs. She’s on steroids now and slowly getting better. I’m not saying stop meds - but ask your doctor: ‘Could this be hurting my kidneys?’ It’s a simple question. Doesn’t make you paranoid. Makes you smart.
Jeremy Butler
December 6, 2025 AT 23:37The ontological implications of pharmacological intervention upon renal homeostasis reveal a profound epistemic rupture between patient agency and biomedical authority. The commodification of symptom suppression, particularly through over-the-counter proton pump inhibitors, constitutes a pathological normalization of physiological neglect - a tacit surrender to the pharmaceutical-industrial complex.
Eric Vlach
December 8, 2025 AT 20:46My dad took naproxen for 15 years for his back. Never thought twice. One day he couldn’t walk. Creatinine was 4.8. He’s on dialysis now. I didn’t know this could happen from OTC stuff. Why isn’t this on every pill bottle? Why isn’t this in every doctor’s office? It’s not just rare - it’s ignored.
Walker Alvey
December 9, 2025 AT 16:28Of course the FDA cares about lawsuits more than your kidneys. They made PPIs require a warning label after 10,000 lawsuits - not because people were dying, but because lawyers got rich. Wake up. The system doesn’t protect you. You have to protect yourself.
Adrian Barnes
December 11, 2025 AT 05:48People who take ibuprofen daily are either ignorant or arrogant. You think you’re being responsible by managing your pain? No. You’re just delaying the inevitable collapse of your renal function. You’re not a patient. You’re a walking liability to the healthcare system.
Patrick Smyth
December 12, 2025 AT 06:08My cousin died from this. She was 42. Took omeprazole for heartburn. Thought it was ‘just heartburn’. She went to bed fine. Woke up with no urine. No one knew. She was gone in 72 hours. I swear to God, if you’re on any of these drugs, get tested. Please. Just get tested.
Linda Migdal
December 12, 2025 AT 17:19AIN is a classic example of pharmacovigilance failure. The cytokine cascade triggered by T-cell infiltration into the renal interstitium is a Type IV hypersensitivity response - not an IgE-mediated allergy. That’s why it’s missed. The diagnostic criteria are underutilized. Eosinophiluria is the key biomarker, yet most ER docs don’t even order it.
Tommy Walton
December 14, 2025 AT 09:19Bro I just took 3 Advil for my headache and now I’m gonna cry about my kidneys 😭肾脏好痛
James Steele
December 15, 2025 AT 10:33The clinical phenomenology of medication-induced interstitial nephritis is an exquisite illustration of the body’s immune system turning inward - a self-immolating response to xenobiotic intrusion. The kidney, as a privileged immune site, becomes the battleground for molecular misrecognition. This is not mere toxicity - it’s immunological betrayal at the tubular level.
Louise Girvan
December 17, 2025 AT 04:53Did you know the FDA is in cahoots with Big Pharma? They only warn about PPIs because they’re running out of lawsuits. The real danger? The vaccines. They cause AIN too. But they won’t tell you that. Your doctor knows. They just won’t say it. Check your blood. Check your urine. They’re watching you.
soorya Raju
December 17, 2025 AT 10:03AIN? More like AIN’t real. I took ibuprofen for 20 years and my kidneys are better than my 30 year old son’s. You people are scared of everything. Next you’ll say breathing is dangerous. Maybe just stop reading fear blogs and go for a walk.