When you’re taking digoxin for heart failure or atrial fibrillation, it’s not just about the pill you swallow each morning. The real danger often comes from what else you’re taking-or eating. Digoxin is a powerful drug with a razor-thin safety margin. Too little, and it won’t help your heart. Too much, and it can trigger dangerous rhythms, nausea, vision changes, or even cardiac arrest. The difference between healing and harm? Often, it’s a simple interaction you didn’t know about.
Why Digoxin Is So Tricky
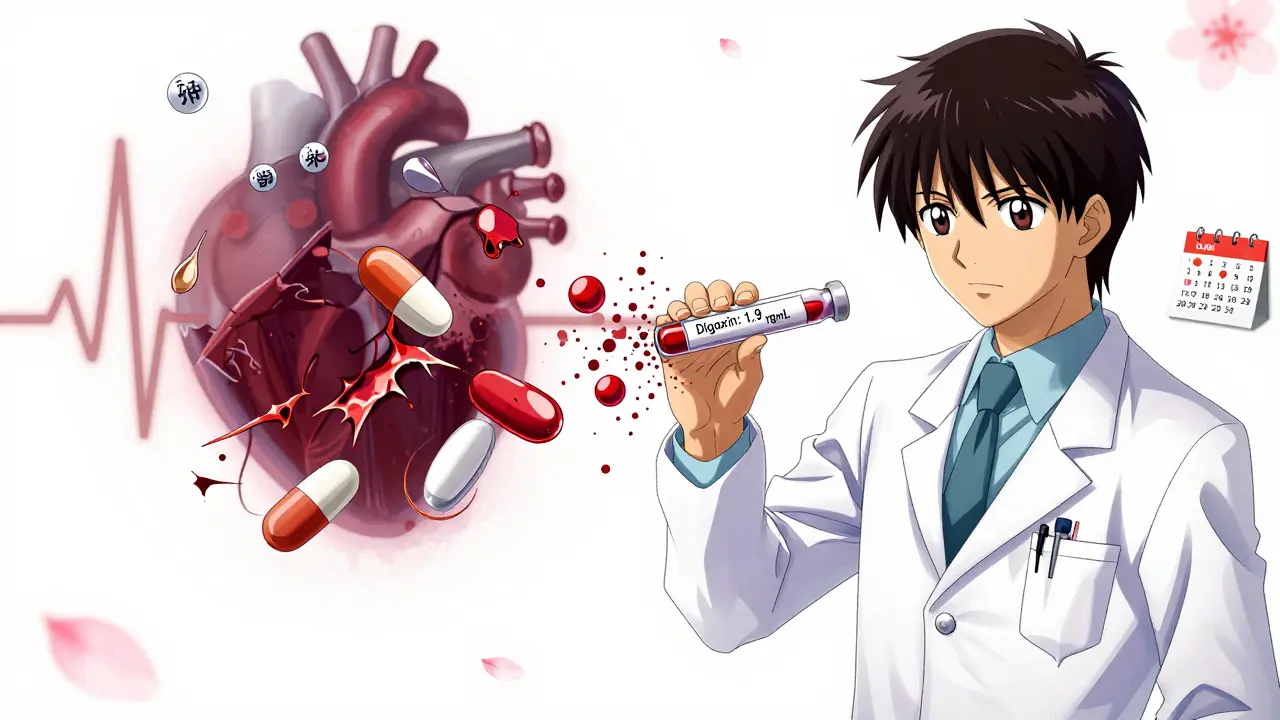
Digoxin works by slowing down your heart rate and helping it pump more strongly. It’s been around since the 1930s, pulled from the foxglove plant. Back then, it was a miracle drug. Today, it’s used more carefully-because we now know how easily it can go wrong. The ideal blood level? Between 0.5 and 0.9 ng/mL. Go above 2.0, and your risk of toxicity spikes. And here’s the catch: you can hit that dangerous level even if you’re taking your exact prescribed dose. Why? Because other drugs, supplements, or even your breakfast can change how your body handles digoxin.
Top 5 Drug Interactions That Can Be Deadly
Some medications mix with digoxin like gasoline and fire. These are the ones you absolutely must tell your doctor about:
- Dronedarone (Multaq): Used for atrial fibrillation, this drug can boost digoxin levels by more than 50%. The PALLAS trial showed patients on both had a 2.5 times higher risk of sudden death. If you’re starting dronedarone, your digoxin dose should be cut in half-with close blood tests for at least two weeks.
- Amiodarone (Cordarone): This antiarrhythmic is common in heart patients, but it can push digoxin levels from safe (0.8 ng/mL) to toxic (1.9 ng/mL) in just two weeks. One patient on the American Heart Association forum described blurred vision and vomiting after starting amiodarone-his levels had skyrocketed.
- Verapamil and Diltiazem: These calcium channel blockers slow your heart rate. Combine them with digoxin, and your pulse can drop below 40 beats per minute. That’s not just dizziness-that’s a risk of needing a pacemaker. The DIONYSOS trial found a 2.7-fold increase in severe bradycardia with this combo.
- Quinidine: This older antiarrhythmic can increase digoxin levels by up to 100% by blocking how your kidneys clear it. It’s rarely used now, but if you’re on it, your digoxin dose needs immediate adjustment.
- Rifampin: An antibiotic used for tuberculosis, rifampin does the opposite-it makes digoxin less effective by speeding up its breakdown. Your levels can drop below therapeutic range, making your heart failure worse without you even knowing.
What You Eat (and Drink) Matters Too
You wouldn’t think oatmeal or licorice could interfere with a heart drug. But they do.
- Black licorice: It contains glycyrrhizin, which pulls potassium out of your body. Low potassium makes digoxin way more toxic-even at normal levels. One study found that just a few ounces of black licorice per day could trigger dangerous heart rhythms in digoxin users. Avoid it completely.
- Oatmeal, high-fiber cereals, and milk: These can reduce digoxin absorption by 20-25%. A Reddit user shared that switching from taking digoxin with breakfast to taking it two hours before eating stabilized his levels. That’s not a myth-it’s science.
- Psyllium fiber supplements: If you take Metamucil or similar, don’t take it within two hours of digoxin. One study showed absorption dropped by 30-40% when taken together.
Supplements That Can Sabotage Your Treatment
Many patients think “natural” means safe. That’s not true with digoxin.
- St. John’s Wort: This popular herb for depression triggers a liver enzyme that flushes digoxin out of your system. Your levels can drop by 25%, making your heart failure worse.
- Hawthorn: Often sold for heart health, hawthorn can lengthen the QT interval on your ECG. Combine it with digoxin, and you risk torsades de pointes-a life-threatening arrhythmia.
- Calcium and magnesium supplements: These can interfere with digoxin absorption if taken at the same time. Space them out by at least two hours.
Diuretics and Electrolytes: The Silent Threat
Most heart patients take diuretics like furosemide (Lasix) or hydrochlorothiazide to reduce swelling. But these drugs make you lose potassium. And low potassium is one of the biggest triggers for digoxin toxicity.
Studies show that about 25% of digoxin users develop hypokalemia (potassium under 3.5 mmol/L). When that happens, even normal digoxin levels become dangerous. That’s why your doctor should check your potassium at least once a month. If it’s low, you may need a potassium supplement-or a switch to a potassium-sparing diuretic like spironolactone.
Who’s at Highest Risk?
Not everyone on digoxin is equally vulnerable. The American College of Cardiology created a simple risk score in 2023 to help doctors spot trouble early:
- Age over 75: +2 points
- Potassium under 4.0: +2 points
- Creatinine over 1.5 (sign of kidney trouble): +2 points
- Digoxin dose over 0.25 mg/day: +1 point
- Taking amiodarone or verapamil/diltiazem: +1 point each
- Body weight under 60 kg: +1 point
If your score is 5 or higher? You’re in the high-risk group. That means weekly blood tests for digoxin levels, not every 3-6 months. It also means your doctor should double-check every new medication-even an over-the-counter antacid.
What About Over-the-Counter Meds?
You’d be surprised how many OTC drugs interfere. Antacids with aluminum or magnesium (like Maalox or Mylanta) can reduce digoxin absorption by up to 30%. A Mayo Clinic study found that 22% of digoxin-related ER visits were tied to these common stomach remedies.
And don’t forget painkillers. While acetaminophen is generally safe, NSAIDs like ibuprofen or naproxen can hurt your kidneys. If your kidneys slow down, digoxin builds up. Stick to acetaminophen for pain, and always check with your pharmacist before taking anything new.
What Should You Do?
Here’s your action plan:
- Take digoxin at the same time every day-preferably on an empty stomach, at least two hours before or after meals.
- Avoid black licorice completely. Read labels on candy, teas, and supplements.
- Keep a list of every medication, supplement, and herb you take. Bring it to every appointment.
- Get your potassium checked monthly. If it’s low, ask your doctor about options.
- Ask your pharmacist: “Does this interact with digoxin?” before taking anything new-even a cold remedy.
- Watch for warning signs: nausea, vomiting, blurred vision, yellow-green halos around lights, or a pulse under 50. Call your doctor immediately.
The Bottom Line
Digoxin isn’t going away. Even though newer drugs exist, it’s still prescribed to 12% of heart failure patients in the U.S.-and up to 35% of those with persistent atrial fibrillation. Why? Because for some people, it works. It’s cheap-often under $6 a month-and it helps when other drugs fall short.
But it’s not a drug you can take on autopilot. It demands attention. Every new pill, every change in diet, every kidney test-it all matters. The goal isn’t to avoid digoxin. It’s to use it safely. With the right monitoring, the right habits, and the right communication with your care team, you can keep your heart strong without putting yourself at risk.
Can I take digoxin with my morning oatmeal?
No. High-fiber foods like oatmeal, bran, and whole grains can reduce digoxin absorption by 20-25%. To ensure your body gets the full dose, take digoxin at least two hours before eating breakfast. Many patients find it easiest to take it right after waking up, before anything else.
What should I do if I miss a dose of digoxin?
If you miss a dose and remember within 12 hours, take it right away. If it’s been more than 12 hours, skip the missed dose and take your next dose at the regular time. Never double up. Digoxin builds up slowly in your system, and taking too much at once can be dangerous.
Can I drink alcohol while taking digoxin?
Moderate alcohol (one drink per day) is usually fine, but heavy drinking can worsen heart failure and increase your risk of arrhythmias. Alcohol can also lower potassium levels and stress your liver and kidneys-both of which affect how digoxin is processed. If you drink, keep it light and talk to your doctor.
How often should digoxin levels be checked?
For stable patients, every 3-6 months is standard. But if you start a new medication, change your dose, or have kidney issues, check every week for the first two weeks. Your doctor should also check potassium and creatinine levels monthly, especially if you’re on diuretics.
Is digoxin safe for elderly patients?
It can be-but with caution. Patients over 75 are nearly three times more likely to experience toxicity. Kidney function naturally declines with age, so digoxin clears more slowly. Doctors often start older patients on lower doses (0.125 mg daily) and monitor closely. Weight matters too: those under 60 kg need even smaller doses.
Can I stop digoxin if I feel better?
No. Even if you feel fine, stopping digoxin suddenly can cause your heart failure symptoms to return quickly. Always talk to your doctor before making any changes. If side effects occur, your doctor may adjust your dose or switch you to another medication-not stop it abruptly.
Are there any new digoxin formulations on the horizon?
Yes. The DIG-FAST trial is testing a new extended-release version that releases digoxin more slowly, reducing spikes in blood levels. Early results suggest it could lower interaction risks by 30%. If approved, it could make digoxin safer for long-term use, especially for patients on multiple medications.
Next Steps for Patients
If you’re on digoxin, schedule a med review with your pharmacist or doctor this week. Bring your pill bottles, supplement labels, and a list of everything you’ve taken in the past month-even “natural” remedies. Ask: “Could any of these be affecting my digoxin?”
Set a monthly reminder to check your potassium level. Keep a small notebook: write down any new symptoms-nausea, dizziness, vision changes-and share them at your next visit. You’re not just a patient. You’re the most important part of your own safety team.

Mussin Machhour
December 25, 2025 AT 23:26Digoxin saved my life after my heart attack, but I had no idea how many things could mess it up. I used to take my pill with oatmeal like everyone told me to-until my grandma, who’s a retired nurse, slapped me upside the head and made me read the label. Now I take it first thing in the morning, water only, and I haven’t had a single weird symptom since. Seriously, if you’re on this drug, treat it like a bomb that only goes off if you do the wrong thing. Don’t be lazy.
Michael Dillon
December 26, 2025 AT 12:50Let’s be real-digoxin is a 1930s relic that shouldn’t even be on the market anymore. Modern drugs like ivabradine and sacubitril/valsartan are safer, more effective, and don’t require a PhD in pharmacology just to avoid poisoning yourself. The fact that doctors still prescribe this like it’s penicillin is criminal negligence. If you’re on digoxin, you’re basically gambling with your heart. And no, ‘it works for me’ isn’t a valid excuse when the data says it kills more people than it saves.
Oluwatosin Ayodele
December 28, 2025 AT 02:15Black licorice? Oatmeal? You people are obsessed with food interactions. The real issue is that most patients don’t get their serum levels checked at all. In Nigeria, we use digoxin daily because it’s cheap and effective-but we check levels weekly because we know the margin is razor-thin. If your doctor isn’t monitoring your digoxin and potassium like a hawk, you’re not being treated-you’re being experimented on. Stop blaming oatmeal. Blame the system that lets you go three months without a blood test.
Jason Jasper
December 28, 2025 AT 23:15I’ve been on digoxin for five years. I take it at 7 a.m. every day, no food for two hours after. I check my pulse every morning. I keep a notebook of every new pill I take-even melatonin. I’m not paranoid. I’m just smart. I’ve seen too many people in the cardiac clinic get admitted because they thought ‘natural’ meant ‘safe.’ My advice? Don’t overthink it. Just be consistent. Take it the same way, every day. And if something feels off? Don’t wait. Call your doctor. It’s not dramatic. It’s survival.
Winni Victor
December 29, 2025 AT 16:02So let me get this straight-I can’t eat licorice, oatmeal, or take my magnesium supplement without risking cardiac arrest? And I’m supposed to trust a drug that’s older than my dad? This isn’t medicine. It’s a Russian roulette game where the bullet is labeled ‘FDA approved.’ I’m switching to CBD oil and prayer. At least then I’m not poisoning myself with a 90-year-old plant extract.
Lindsay Hensel
December 31, 2025 AT 14:17Thank you for this meticulously researched and clinically grounded exposition. The clarity with which you delineate the pharmacokinetic interactions of digoxin is both rare and deeply appreciated in today’s era of algorithm-driven health misinformation. I shall immediately schedule a medication review with my pharmacist and ensure monthly electrolyte monitoring is documented in my care plan. Your guidance is not merely informative-it is life-preserving.
Sophie Stallkind
January 2, 2026 AT 11:35I have been on digoxin for over a decade. I take it at the same time every day, always on an empty stomach. I avoid all fiber supplements within two hours. I check my potassium levels every month. I do not take any new medication without consulting my cardiologist. I do not use herbal remedies. I do not consume licorice. I have never experienced toxicity. This is not luck. This is discipline. If you are on digoxin, you owe it to yourself to be this careful.
Katherine Blumhardt
January 2, 2026 AT 22:38Ok so i just started digoxin and i was like wait does this mean i cant eat my morning granola? and also my mom gave me that hawthorn tea for ‘heart health’ and now im like oh no oh no oh no. also i think my pharmacist is judging me when i ask if tylenol is ok. i just want to live and not die from oatmeal. help.
Linda B.
January 4, 2026 AT 19:47They don’t want you to know this but digoxin was never meant for humans. It was developed by Big Pharma to keep seniors dependent on monthly blood tests and expensive labs. The real reason they still prescribe it? Because Medicare pays for it and nobody wants to admit the truth-that it’s a money-making trap wrapped in a 90-year-old myth. Watch your levels? Sure. But watch who’s profiting from your fear even more.
Christopher King
January 4, 2026 AT 22:44EVERYTHING is a conspiracy. The FDA? Controlled. The doctors? Paid off. Even your oatmeal? Probably laced with glyphosate to make digoxin more toxic so you’ll keep going back for more blood tests. The foxglove plant? It knew. It warned us. It whispered through the wind. And yet-you still eat your breakfast. You still take your pill. You still trust the system. You’re not a patient. You’re a pawn. Wake up. The truth is in the silence between your heartbeat.
Bailey Adkison
January 6, 2026 AT 07:43Correction: The DIONYSOS trial showed a 2.7-fold increase in severe bradycardia with verapamil/diltiazem and digoxin-not ‘nearly three times’ as some lazy blogs claim. Also, psyllium reduces absorption by 30–40% only when taken simultaneously. If you space them by two hours, the effect is negligible. Stop exaggerating. Precision matters. Your life depends on it.
Gary Hartung
January 6, 2026 AT 18:46Let’s be honest-digoxin is the last gasp of the medical establishment’s refusal to evolve. It’s like prescribing leeches for hypertension. The fact that you’re being told to ‘monitor your potassium’ like it’s a yoga practice instead of a critical biomarker? That’s not medicine. That’s medieval theater. And the fact that you’re nodding along, taking notes, and calling it ‘empowerment’? That’s the real tragedy. You’re not safe. You’re just conditioned.