Getting the right dose of medication isn’t just about following the label. For many people, especially older adults, those with chronic conditions, or people who are underweight or overweight, the standard dose can be too much-or too little. Too high, and you risk toxicity. Too low, and the drug doesn’t work. That’s why medication dosing must be adjusted based on age, weight, and kidney function. These aren’t optional tweaks-they’re essential for safety.
Why One Size Doesn’t Fit All
Think of your body like a car. A 10-year-old sedan and a brand-new sports car don’t use fuel the same way, even if they’re the same make. Your body processes drugs the same way. As you age, your kidneys slow down. If you carry extra weight, your body holds drugs differently. And if your kidneys aren’t working well, drugs build up in your blood instead of being cleared out. The result? A 70-year-old woman with Stage 3 kidney disease might need half the dose of a 35-year-old man with healthy kidneys-even if they have the same diagnosis. Ignoring these differences is one of the leading causes of preventable hospital admissions in older adults.How Kidney Function Changes Everything
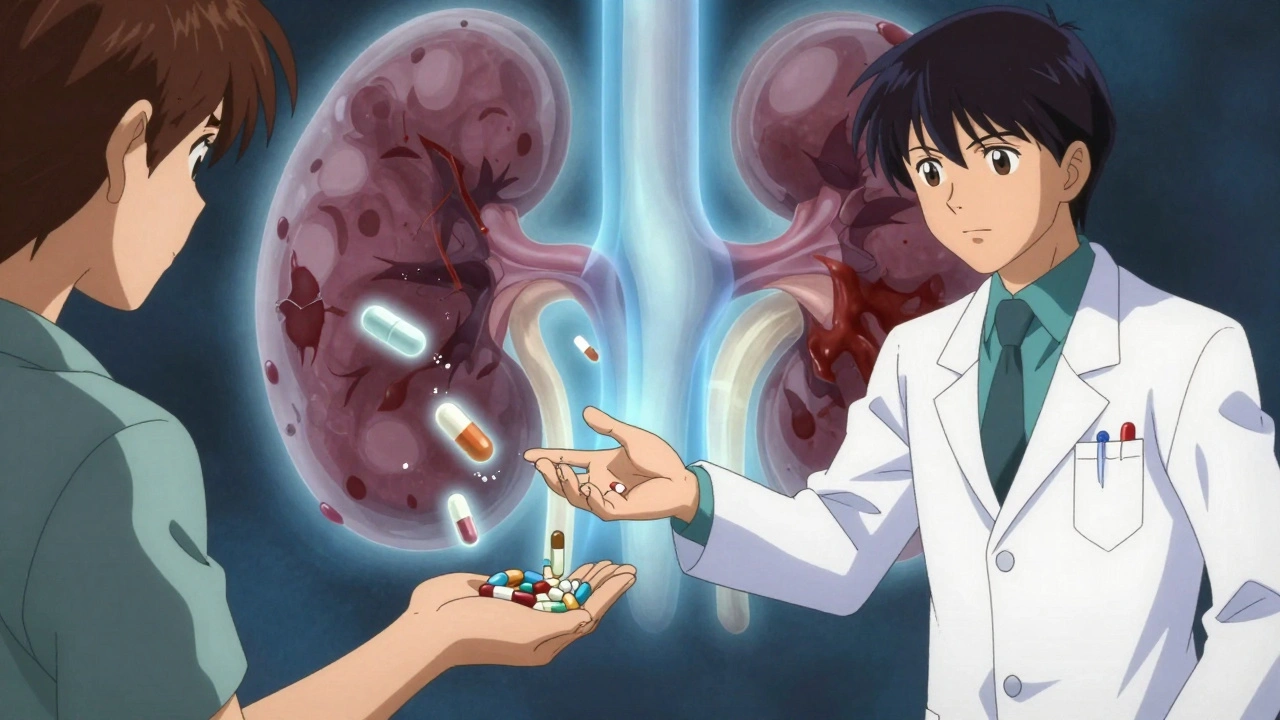
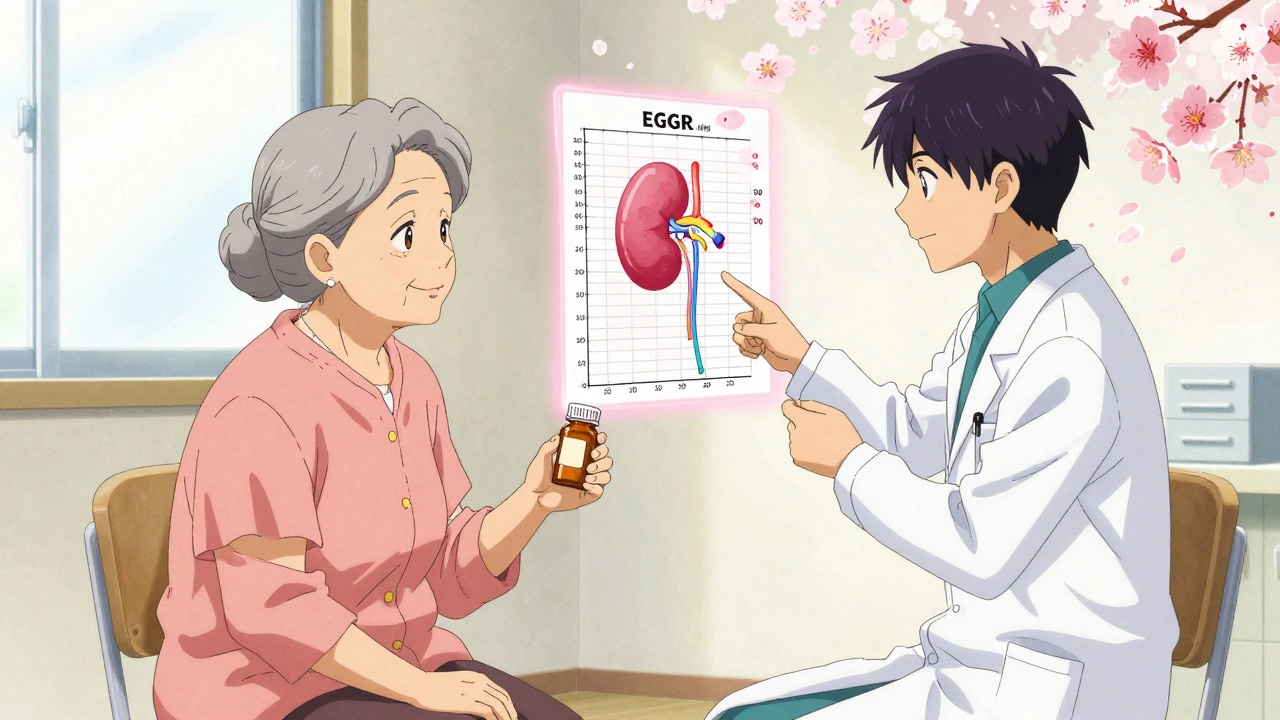
Your kidneys are the main filters for most medications. When they’re healthy, they clear drugs efficiently. When they’re not, those drugs stick around-and can become toxic. Doctors don’t just look at your serum creatinine level. They calculate your estimated glomerular filtration rate (eGFR), which tells them how well your kidneys are filtering waste. The CKD-EPI equation is now the standard for this. It uses your age, sex, race, and creatinine level to estimate kidney function. Here’s how kidney stages affect dosing:- eGFR ≥90: Normal function. No adjustment needed for most drugs.
- eGFR 60-89: Mild reduction. Some drugs may need small changes.
- eGFR 30-59: Moderate reduction (Stage 3). Many drugs require dose reduction or longer dosing intervals.
- eGFR 15-29: Severe reduction (Stage 4). Most renally cleared drugs need major adjustments.
- eGFR <15: Kidney failure (Stage 5). Often requires complete avoidance or dialysis-based dosing.
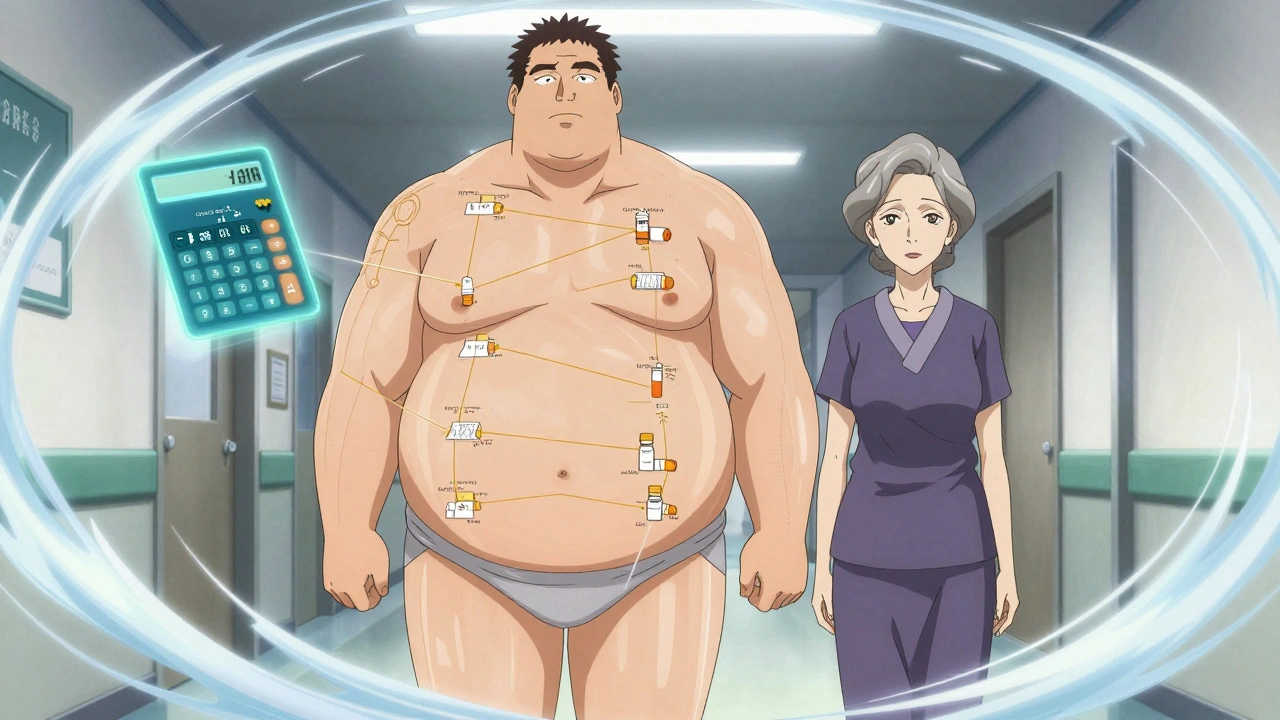
Weight Matters More Than You Think
If you’re obese, your body doesn’t just have more fat-it has more fluid and different tissue distribution. Many drugs dissolve in water, not fat. So if you’re overweight, giving a dose based on your actual weight can lead to overdose. That’s why doctors use adjusted body weight for dosing:- For men: Ideal Body Weight (IBW) = 50 kg + 2.3 kg for each inch over 5 feet
- For women: IBW = 45.5 kg + 2.3 kg for each inch over 5 feet
- Adjusted weight = IBW + 0.4 × (actual weight − IBW)
Age Isn’t Just a Number
People over 65 are more likely to have reduced kidney function-even if their creatinine looks normal. Muscle mass declines with age, so creatinine production drops. That makes eGFR look better than it really is. A 75-year-old woman with a creatinine of 1.1 mg/dL might seem to have normal kidney function. But if she’s lost muscle, her true GFR could be below 45 mL/min. That’s Stage 3 kidney disease. Giving her a full dose of a drug like metformin or vancomycin could be dangerous. Studies show that 30% of adverse drug events in older adults are due to incorrect dosing in kidney impairment. And it’s not just about kidneys. Liver function, brain sensitivity to sedatives, and changes in how drugs bind to proteins all shift with age.What Drugs Need the Most Attention?
Not every medication needs adjustment. But some are high-risk:- Metformin: Must be stopped if eGFR falls below 30. Dose must be reduced at eGFR 30-45.
- Vancomycin: Dosing is based on CrCl. Underdosing leads to treatment failure; overdosing causes hearing loss or kidney damage.
- NSAIDs (ibuprofen, naproxen): Can worsen kidney function and raise blood pressure. Avoid in Stage 3 or worse.
- ACE inhibitors and ARBs: Often used in kidney disease-but need dose reduction and close monitoring.
- Antibiotics (cefazolin, ciprofloxacin): Many are cleared by kidneys. Dosing varies wildly between guidelines.
- Antidepressants and antipsychotics: Accumulate in elderly patients, increasing fall risk and confusion.
Real-World Mistakes (And How to Avoid Them)
Here’s what goes wrong in practice:- A 72-year-old with eGFR 28 gets 1,000 mg of metformin twice daily. The FDA says max is 500 mg daily. She ends up in the ER with lactic acidosis.
- A 90 kg man with Stage 3 CKD gets a full dose of cefazolin. His CrCl is only 40 mL/min. He develops seizures from drug buildup.
- A thin 80-year-old woman gets a standard dose of morphine. She’s sedated for 48 hours.
Technology Is Helping-But Not Perfect
Most hospitals now have electronic alerts that flag when a dose might be wrong for kidney function. One study showed these alerts cut medication errors by 47%. But alerts can be ignored or wrong. Some systems use eGFR for dosing recommendations, even though guidelines were built on CrCl. Others don’t account for obesity or underweight. A 2023 study found 38% of antibiotic dosing guidelines had conflicting recommendations across different sources. The best systems combine CrCl calculation, adjusted weight, and drug-specific rules. They don’t just say “reduce dose.” They say “reduce to 50% every 24 hours” or “switch to non-renal alternative.”What You Can Do
You don’t need to calculate CrCl yourself-but you can be an active partner in your care:- Know your eGFR. Ask your doctor for your latest number.
- Keep a list of all your medications-including over-the-counter and supplements.
- Ask: “Is this dose right for my kidneys and my weight?”
- If you’re over 65 or have diabetes, high blood pressure, or heart disease, assume your kidneys aren’t perfect until proven otherwise.
- Bring your medication list to every appointment. Don’t assume your doctor remembers what you were on last time.
The Bottom Line
Medication dosing isn’t just about what’s on the bottle. It’s about who you are-your age, your weight, your kidney health. A dose that’s safe for one person could be deadly for another. The science is clear. The tools exist. What’s missing is consistent application. The goal isn’t to overcomplicate things. It’s to make sure every pill you take works as it should-without harming you. That means asking questions, checking your numbers, and trusting your pharmacist. Because when it comes to your health, the right dose isn’t a suggestion. It’s a necessity.How do I know if my medication dose needs to be adjusted for kidney function?
Your doctor should check your estimated glomerular filtration rate (eGFR) at least once a year if you’re over 60, have diabetes, high blood pressure, or heart disease. If your eGFR is below 60 mL/min/1.73m², ask if any of your medications need a dose change. Common drugs like metformin, vancomycin, and NSAIDs almost always require adjustment at this level.
Can I use my actual weight to calculate my dose if I’m overweight?
No-not for most medications. If your BMI is over 30, using your actual weight can lead to overdose. Doctors use adjusted body weight: Ideal Body Weight + 40% of the difference between your actual weight and ideal weight. This prevents giving too much drug to your fat tissue, which doesn’t absorb most medications well.
Why do some sources say to use Cockcroft-Gault and others say to use CKD-EPI?
CKD-EPI is better for diagnosing kidney disease and staging it. But most drug dosing guidelines were developed using the Cockcroft-Gault equation, which estimates creatinine clearance (CrCl) instead of eGFR. For dosing, CrCl is still the standard. So even if your lab reports eGFR, your doctor may need to calculate CrCl using Cockcroft-Gault to get the right dose.
What should I do if I’m told to stop a medication because of my kidney function?
Don’t stop it on your own. Some drugs, like blood pressure medications, are actually protecting your kidneys-even if your function is low. Ask your doctor if there’s a safer alternative. For example, metformin might be switched to a non-renal drug like dapagliflozin. Never assume stopping is the only option.
Are there any tools or apps that help with dosing calculations?
Yes. Many hospitals use integrated systems like Epic or Cerner that auto-calculate CrCl and flag unsafe doses. For personal use, trusted apps like Micromedex or Lexicomp (available through some pharmacies) provide dosing guidelines. Avoid random online calculators-they often use outdated formulas or don’t account for obesity or age.
Ignacio Pacheco
December 3, 2025 AT 17:52So let me get this straight - we’re using a 1970s formula (Cockcroft-Gault) to dose modern meds because the FDA didn’t update their guidelines when eGFR became the gold standard? That’s not clinical practice, that’s bureaucratic archaeology.
And don’t even get me started on how hospitals still use CrCl in their EHR alerts while the lab reports eGFR. It’s like giving someone a GPS that only works with paper maps.
Meanwhile, pharmacists are the only ones still reading the actual prescribing info. The rest of us are just hoping the computer doesn’t kill us.
Also - why is metformin still on the market? It’s basically a slow-acting poison if your kidneys blink wrong. Someone should just make a non-renal metformin. Or ban it. Either way.
And yes, I’m the guy who printed out the dosing tables and taped them to my fridge. Don’t judge me.
sagar bhute
December 3, 2025 AT 19:47This article is a joke. In India we don’t have access to eGFR tests for 90% of patients. We use creatinine and guess. You think a poor diabetic in rural Bihar is getting adjusted weight calculations? They get whatever the pharmacy has left. This is rich people medicine dressed up as science.
Stop pretending this is about safety. It’s about profit. Pharma companies don’t want to retest drugs for every body type. They want one dose for everyone so they can sell more pills.
And don’t even mention ‘trust your pharmacist’ - in my town, the pharmacist doesn’t know what metformin is. He just hands out the bottle and says ‘take two.’
shalini vaishnav
December 4, 2025 AT 00:43How can Americans still be this naive? You have the most advanced medical system in the world - and yet you’re still using outdated equations because ‘that’s how it’s always been done’? This is why your healthcare costs are insane. You over-test, over-calculate, and still get it wrong.
In India, we don’t waste time with adjusted body weight formulas. We use actual weight, monitor the patient, and adjust as needed. Simple. Efficient. No bureaucracy. No apps. No alerts. Just clinical judgment.
And your obsession with ‘eGFR’? Please. Creatinine is enough. Your kidneys don’t care about race corrections. That’s just data colonialism.
Stop overcomplicating what should be basic medicine.
Vincent Soldja
December 4, 2025 AT 10:16Too long. Didn’t read.
Just give me the pill.
And don’t ask me about my kidneys.
I’m fine.
Chloe Madison
December 5, 2025 AT 18:38Hey - if you’re reading this, you’re already ahead of 90% of patients. Seriously.
Knowing your eGFR? Asking about dosing? Bringing your med list to appointments? That’s not just smart - that’s life-saving behavior.
And if your doctor brushes you off? Go to the pharmacy. Ask the pharmacist. They’re the unsung heroes of medication safety. Most of them know your meds better than your doctor does.
Don’t wait for an alert. Don’t wait for a study. Ask the question now. Even if it feels awkward. Even if they roll their eyes.
Your body isn’t a one-size-fits-all machine. And you deserve care that matches who you actually are - not who the algorithm thinks you are.
Gavin Boyne
December 7, 2025 AT 12:09Let’s be real - the entire system is a joke. We’ve got AI that can predict cancer from a retinal scan, but we still rely on a 50-year-old formula to tell us how much insulin to give an 80-year-old woman with 30% kidney function?
And don’t get me started on the ‘race correction’ in eGFR. That’s not science. That’s 19th-century racism wrapped in a lab coat.
Meanwhile, my cousin in Ohio got a full dose of vancomycin because the computer said ‘normal creatinine.’ She ended up with permanent hearing loss. The hospital apologized. Sent her a $50 gift card.
So yeah. We’re not just underdosing or overdosing.
We’re failing people systematically.
And the worst part? We all know it. And we keep doing it anyway.
Because change is hard.
And profit is easier.
Gene Linetsky
December 8, 2025 AT 07:41Wait - so you’re telling me the government and Big Pharma are hiding the truth about kidney dosing? And that’s why so many old people end up in the ER? And that’s why the CDC won’t admit it?
Look - I’ve seen the documents. The FDA knew. The drug reps knew. But they didn’t change the labels because it would cost too much to retest.
And now they’re pushing eGFR to distract us from the real issue: they don’t want to pay for individualized dosing.
They want you to take the same pill as your neighbor - even if you’re 60 pounds lighter and have diabetes.
It’s not incompetence.
It’s criminal.
And they’re still selling it as ‘evidence-based.’
Jim Schultz
December 9, 2025 AT 08:17Okay, so here’s the thing: I’ve been a pharmacist for 22 years, and I’ve seen this exact scenario play out 1,000 times.
Older patient. Normal creatinine. Normal eGFR. But muscle mass? Gone. Kidney function? Half of what the numbers say.
They get metformin. They get vancomycin. They get NSAIDs. And then they crash.
And guess who gets blamed? The patient. ‘Why didn’t you tell us you were dizzy?’ ‘Why didn’t you stop the pills?’
Meanwhile, the prescriber didn’t check CrCl. Didn’t adjust for weight. Didn’t consult the pharmacist.
And now? The system is broken.
Not because of science.
Because of time.
Because doctors have 7 minutes per patient.
And no one has time to think.
So we keep doing the same thing.
And people keep dying.
And we call it ‘standard of care.’
That’s not care.
That’s negligence dressed in a white coat.