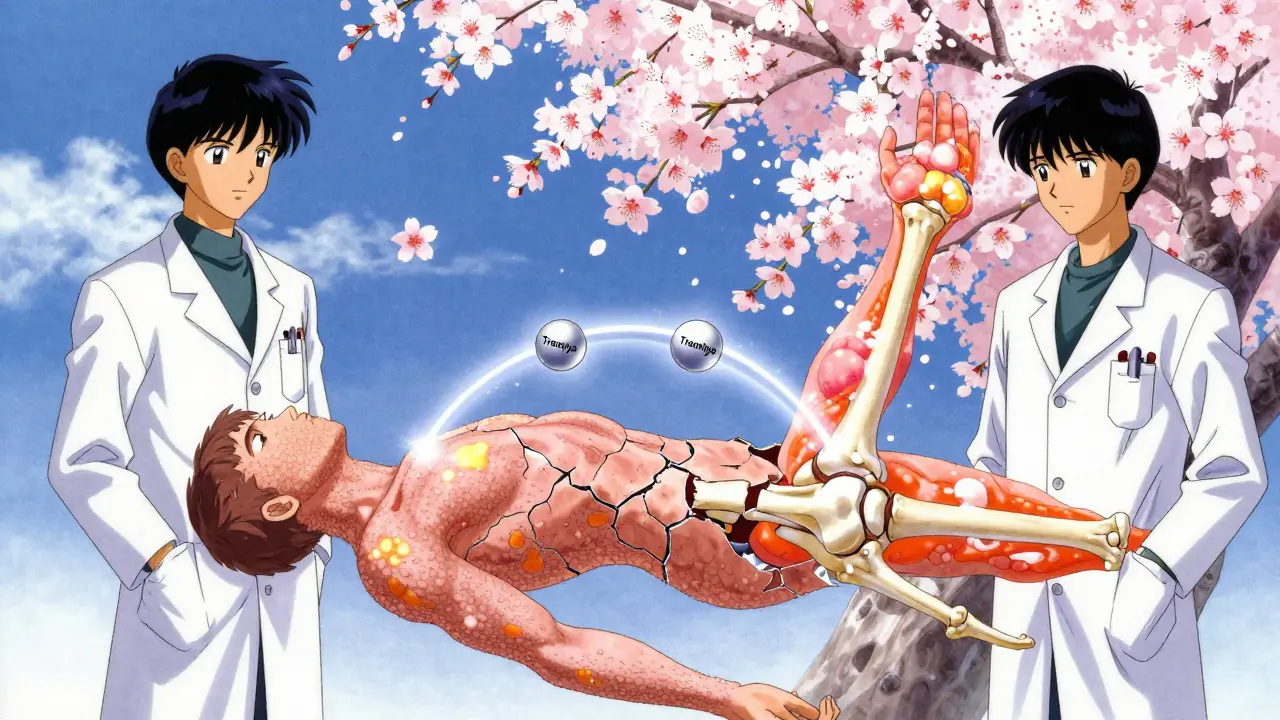
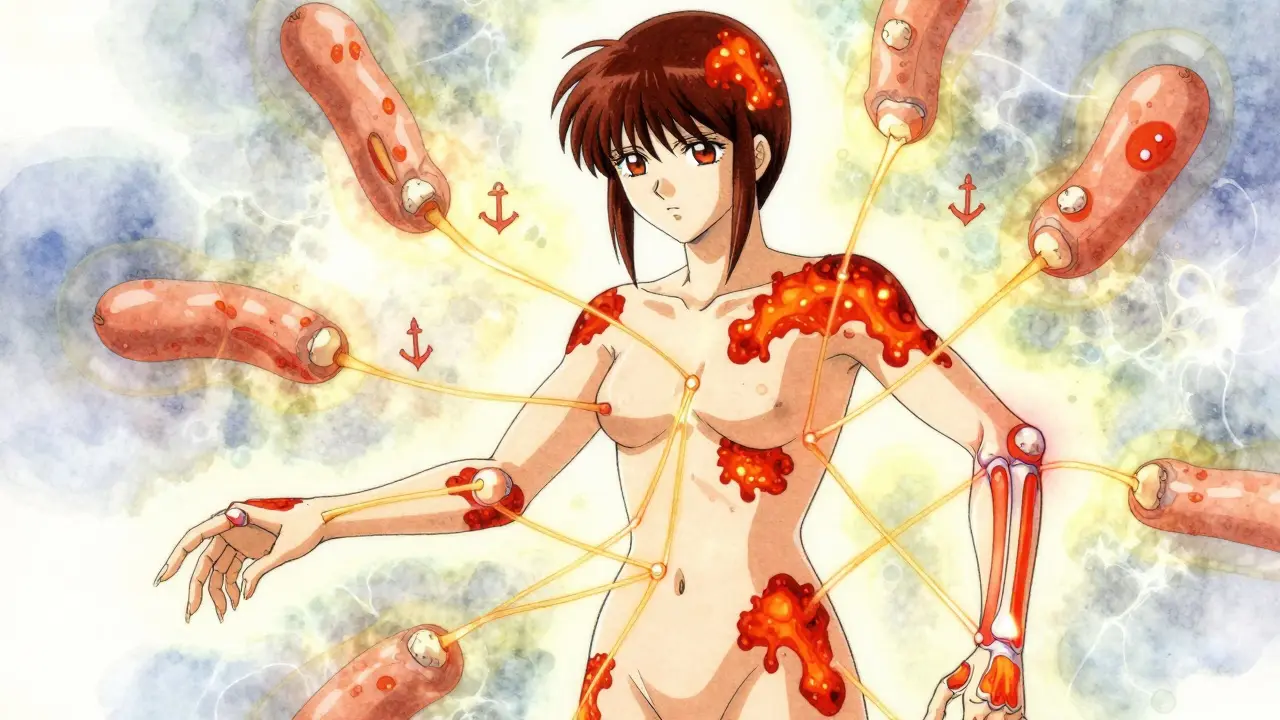
When your skin breaks out in red, scaly patches and your fingers or toes suddenly swell up like sausages, it’s not just coincidence. These aren’t two separate problems-they’re two signs of the same hidden disease: psoriatic arthritis. For years, many people thought psoriasis and joint pain were unrelated. But the truth is, your skin and joints are talking to each other-and your immune system is the one doing the shouting.
How Your Skin and Joints Are Connected
Psoriatic arthritis doesn’t just happen to people with psoriasis. It’s the same immune system mistake causing both. Your body’s defenses go haywire and start attacking healthy tissue-first in the skin, then in the joints, tendons, and even your nails. About 30% of people with plaque psoriasis will develop psoriatic arthritis. And while most get skin symptoms first, 15% actually feel joint pain before any rash appears. The inflammation doesn’t stay in one place. It spreads from the skin’s outer layers down into the synovium-the lining of your joints-and into the entheses, where tendons and ligaments attach to bone. That’s why you might have painful heels (plantar fasciitis), swollen fingers, or a stiff lower back. The same immune signals that cause flaky skin on your elbows also trigger swelling in your knees.Signs You Might Have Psoriatic Arthritis
If you have psoriasis and notice any of these, don’t wait:- Swollen fingers or toes - not just a little puffiness, but full, sausage-like swelling called dactylitis. This happens in nearly half of all cases.
- Nail changes - pits, ridges, or your nail lifting off the nail bed (onycholysis). Eight out of ten people with psoriatic arthritis have this.
- Asymmetric joint pain - your right knee aches, but your left knee doesn’t. That’s different from rheumatoid arthritis, which usually hits both sides evenly.
- Stiffness that lasts - not just morning stiffness that fades after 15 minutes. This sticks around for over an hour and doesn’t improve with movement alone.
- Pain where tendons attach - achy heels, sore elbows, or a stiff neck. This is called enthesitis and shows up in up to 40% of patients.
Five Types of Psoriatic Arthritis
This isn’t one-size-fits-all. Doctors see five main patterns:- Asymmetric oligoarthritis - affects fewer than five joints, often in different areas. This is the most common type, seen in 70% of cases.
- Symmetric polyarthritis - looks like rheumatoid arthritis, with matching joints on both sides. About 25% of people have this.
- Distal interphalangeal predominant - mainly hits the joints closest to your fingernails and toenails. Only 5% of cases, but very telling if present.
- Spondylitis - affects your spine and neck. Happens in 5-20% of people. Can feel like regular back pain, but doesn’t improve with rest.
- Arthritis mutilans - the rarest and most severe. Destroys small bones in hands and feet. Less than 5% of cases, but can cause permanent deformity.
Why Diagnosis Takes So Long
The average person waits over two years to get diagnosed. Why? Because there’s no single blood test. Unlike rheumatoid arthritis, where the rheumatoid factor shows up in most patients, 90% of psoriatic arthritis cases test negative. Doctors rely on signs: your skin, your nails, your joint pattern, and imaging. Many people are misdiagnosed with osteoarthritis or rheumatoid arthritis first. A Reddit user shared how they were treated for rheumatoid arthritis for five years before a dermatologist spotted the nail pitting and connected the dots. That’s why seeing both a dermatologist and a rheumatologist matters. Nearly half of psoriatic arthritis cases are first spotted by skin doctors, not joint specialists.Treatments That Actually Work
There’s no cure-but you can stop the damage. The goal isn’t just to feel better. It’s to prevent permanent joint destruction. Studies show that starting treatment within 12 weeks of symptoms cuts the risk of lasting damage by 75%. Here’s what works:- DMARDs - like methotrexate. These slow down the immune system broadly. Often used first, but not always enough on their own.
- Biologics - these are targeted shots or infusions that block specific inflammation signals. TNF inhibitors like adalimumab (Humira) and etanercept (Enbrel) were the first breakthroughs. Newer ones like guselkumab (Tremfya) and ustekinumab (Stelara) target different pathways and often work better for skin and joints together.
- Oral JAK inhibitors - like upadacitinib. These are pills, not injections, and are showing strong results in trials expected to be approved by late 2024.
- TYK2 inhibitors - deucravacitinib (Sotyktu), approved in 2022, is the first in its class. It works on a different immune pathway and helps both skin and joints without suppressing your whole system.
What Doesn’t Work (And Why)
Painkillers like ibuprofen might ease discomfort, but they don’t stop the disease. Steroid injections help temporarily, but they’re not a long-term fix. And if you’re told your joint pain is “just aging,” push back. Psoriatic arthritis doesn’t wait. Many people stop treatment because of side effects or cost. Biologics can cost over $500 a month out-of-pocket. Insurance approvals take nearly three weeks on average. But skipping doses or stopping treatment lets inflammation creep back-and that’s when joint damage happens fast.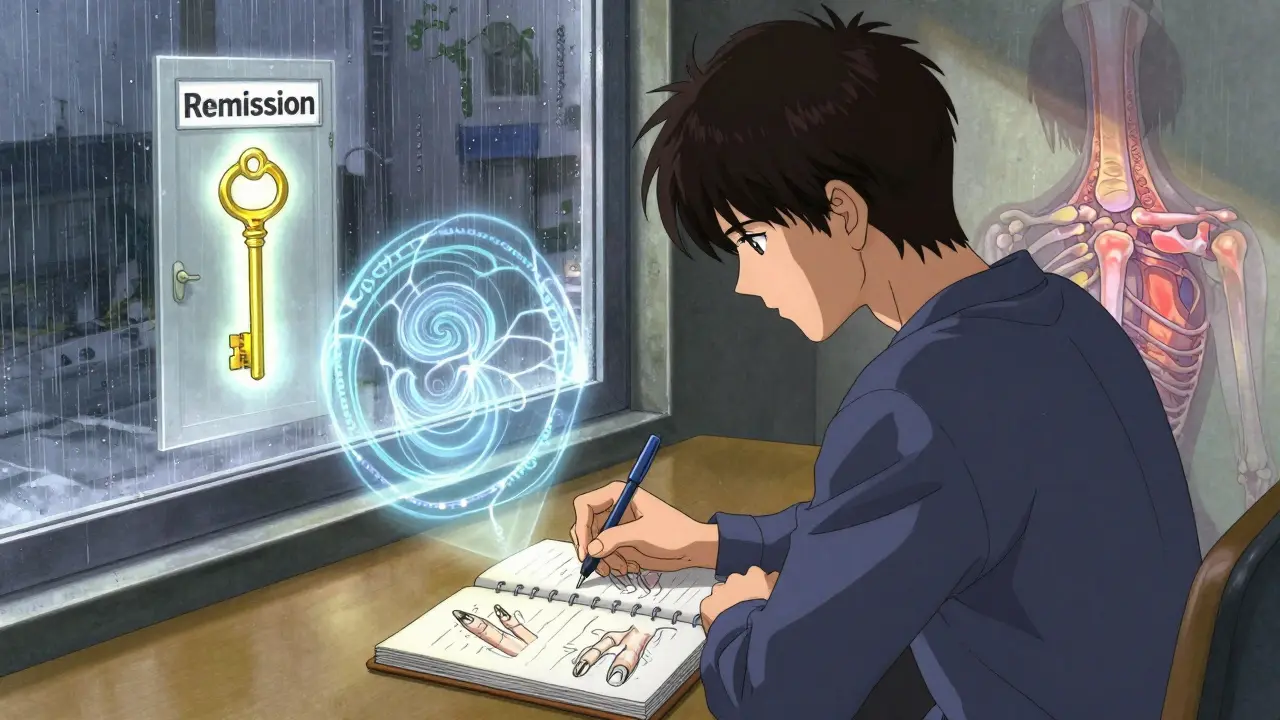
Living With It: Daily Strategies
Treatment is only half the battle. How you live matters too:- Move gently - physical therapy isn’t optional. Low-impact exercise like swimming or cycling keeps joints mobile without wrecking them.
- Track your triggers - stress, infections, alcohol, or even weather changes can spark flares. Most people figure out their triggers after 3-6 months of journaling.
- Protect your nails - avoid biting them or using harsh nail polish removers. Nail health is a direct window into your disease activity.
- Manage fatigue - it’s not laziness. Inflammation drains your energy. Prioritize sleep and rest breaks.
- Get screened - before starting biologics, you need TB and hepatitis tests. It’s not a formality-it’s safety.
The Future Is Personalized
The next big shift? Personalized treatment. Researchers are using AI to predict who’ll develop psoriatic arthritis from their psoriasis-based on nail scans and joint imaging-with 87% accuracy. By 2028, genetic testing may tell you which drug will work best for you, cutting out the trial-and-error phase. Right now, patients try an average of 2.3 different drugs before finding one that works. That’s changing. New drugs are coming fast, and the global market for treatments is expected to nearly double by 2030.What You Need to Do Now
If you have psoriasis and joint pain, swelling, or stiffness:- See a rheumatologist-not just your GP.
- Bring photos of your skin and nail changes.
- Ask: “Could this be psoriatic arthritis?”
- Insist on early treatment. Delaying risks permanent damage.
- Work with both a dermatologist and a rheumatologist. Coordination matters.
Can psoriatic arthritis develop without skin psoriasis?
Yes, but it’s rare. About 15% of people develop joint symptoms before any visible skin rash appears. This makes diagnosis harder, but if you have a family history of psoriasis or nail changes, doctors will still suspect psoriatic arthritis. Skin changes may appear later, so ongoing monitoring is key.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. Rheumatoid arthritis usually affects joints symmetrically (both hands, both knees) and shows positive blood markers like rheumatoid factor. Psoriatic arthritis is often asymmetric, involves entheses and nails, and typically has negative blood tests. Dactylitis and skin plaques are unique to psoriatic arthritis.
Do biologics cure psoriatic arthritis?
No, but they can put the disease into remission. Biologics stop the immune system from attacking your joints and skin. Many people achieve minimal disease activity and can live without joint damage. Stopping treatment often leads to flare-ups, so most need to stay on them long-term.
Can diet or supplements help psoriatic arthritis?
No diet or supplement has been proven to stop psoriatic arthritis progression. However, maintaining a healthy weight reduces joint stress, and some people report less inflammation with anti-inflammatory diets (rich in fish, vegetables, nuts). Omega-3s and vitamin D may help with general health, but they’re not replacements for medical treatment.
How long does it take for psoriatic arthritis treatments to work?
It varies. DMARDs like methotrexate can take 6-12 weeks. Biologics like Tremfya or Stelara often show improvement in 4-12 weeks. Some people feel better in days with newer drugs, but full effect can take months. Patience is key, but if there’s no change after 3 months, talk to your doctor about switching.
Is psoriatic arthritis hereditary?
Yes, genetics play a strong role. If a parent or sibling has psoriasis or psoriatic arthritis, your risk increases. Around 40% of people with the condition have a close relative with it. But having the genes doesn’t mean you’ll get it-environmental triggers like stress, infection, or injury often start the disease.
Can psoriatic arthritis affect organs other than joints and skin?
Yes. Chronic inflammation raises your risk for heart disease, fatty liver disease, and metabolic syndrome. People with psoriatic arthritis have a 1.5 times higher risk of heart attack than the general population. Regular heart health checks are part of long-term management.
What happens if I ignore my joint pain?
Without treatment, up to 30% of people develop irreversible joint damage within two years. This can lead to deformities, loss of function, and disability. Early treatment stops this. Waiting doesn’t make the disease milder-it makes it harder to control.
Adewumi Gbotemi
January 12, 2026 AT 06:18Man, I never realized my nail pits and swollen fingers were linked. I thought it was just old age and dry skin. This post literally changed how I see my body. Gonna book a dermatologist next week.
Thanks for laying it out so simple.
Sean Feng
January 12, 2026 AT 23:49So basically your immune system is just a drunk roommate who keeps punching the walls and then blames the carpet
Great article though
Jason Shriner
January 14, 2026 AT 21:10Oh wow. So instead of just accepting that life is pain and your body is a glitchy android, we now have $500/month injections to make it slightly less miserable.
Capitalism really outdid itself this time. Next up: biologics for existential dread.
Also, my cat has better insurance than I do.
Sam Davies
January 15, 2026 AT 03:00Let’s be real - psoriatic arthritis isn’t a disease, it’s a lifestyle brand now. You’ve got your Tremfya influencers, your Stelara yoga retreats, your dactylitis merch. I’m just waiting for the podcast: ‘Skin, Sausage Fingers & Serotonin’.
Still, the science is legit. Just… why does everything now require a subscription?
Alex Smith
January 15, 2026 AT 23:51People who say ‘just lose weight’ or ‘try turmeric’ need to stop. This isn’t a Pinterest hack - it’s systemic autoimmunity.
And yes, I’ve seen the guy who swears his ‘anti-inflammatory smoothie’ cured his enthesitis. Bro. Your knees still look like overcooked hot dogs.
Do the science. Get the tests. Don’t let your GP gaslight you into thinking it’s ‘just aging’.
Roshan Joy
January 16, 2026 AT 20:06Been living with this for 8 years. Started with just a flaky elbow, then one toe swelled up like a sausage 🥲
Stelara changed my life. Took 3 months but now I can hold my kid without wincing. Also, tracking triggers with an app helped me avoid 70% of flares.
Don’t give up. You’re not alone. 💪❤️
Michael Patterson
January 17, 2026 AT 04:37Look, I read this whole thing and I’m still not convinced this isn’t just a fancy name for ‘your body hates you’. You got psoriasis? Fine. You got joint pain? Fine. But linking them? That’s like saying ‘my sneeze caused my toenail fungus’. Correlation isn’t causation, bro. And don’t even get me started on biologics - you think a $60k drug is gonna fix your immune system’s bad day? You’re just feeding Big Pharma. Also, typo: ‘synovium’ is spelled wrong in paragraph 3. And why are you telling me about nail polish removers like I’m a 12-year-old girl?
Also, your ‘five types’ chart is just a marketing brochure. Real doctors don’t care about labels. They care about pain levels and mobility. End of story.
Matthew Miller
January 17, 2026 AT 05:22Pathetic. You people actually think a pill or a shot fixes this? You’re just delaying the inevitable. Your immune system is broken. No drug in the world fixes that. You’re just buying time while your joints rot and your skin peels off like wallpaper. And now you’re gonna spend your life begging insurance companies for coverage? Congrats. You’ve won the genetic lottery. The real treatment? Accept that you’re broken. And stop pretending science is gonna save you.