Drug Interaction Safety Checker
Check for Dangerous Interactions
Enter your medications to see if they could interact dangerously. Include all prescription drugs, OTC medications, and supplements.
Imagine taking two common medications - one for your cholesterol, another for an infection - and not realizing they could shut down your muscles, damage your kidneys, or even stop your heart. This isn’t science fiction. It’s happening in pharmacies across the country, every single day. And the people who are supposed to catch it - your pharmacist - are often overwhelmed, distracted, or trained to ignore the very alerts meant to save lives.
Why Some Drug Combinations Are Deadly
Not all drug interactions are the same. Some cause mild nausea. Others cause death. The most dangerous ones happen when two medications interfere with how your body breaks them down. This usually involves enzymes in your liver, like CYP3A4 or CYP2C9, or transporters like P-glycoprotein. When one drug blocks or speeds up these systems, the other can build up to toxic levels - or vanish before it can work. Take simvastatin and clarithromycin. Simvastatin lowers cholesterol. Clarithromycin fights bacterial infections. Together, they can trigger rhabdomyolysis - a condition where muscle tissue breaks down so fast that it floods your kidneys with toxins. Studies show creatine kinase levels can spike to 10,000 U/L in severe cases. Normal is under 200. Without intervention, this leads to kidney failure, dialysis, or death. Another deadly pair: colchicine (for gout) and verapamil (for high blood pressure). Verapamil blocks the P-glycoprotein transporter that normally flushes colchicine out of your body. The result? Colchicine builds up to lethal levels. There have been documented cases of patients dying from multi-organ failure after just a few days of this combo. Even something as simple as an antibiotic and a muscle relaxer can be deadly. Tizanidine + ciprofloxacin inhibits the CYP1A2 enzyme, causing tizanidine levels to skyrocket. Patients have passed out, fallen, fractured bones, and ended up in the ER - all because no one checked the interaction.The Forgotten Warning: Birth Control and Antifungals
Some interactions don’t kill you - they change your life. Norgestimate/ethinyl estradiol (a common birth control pill) combined with griseofulvin (an antifungal for nail fungus) can render contraception useless. Why? Griseofulvin boosts CYP3A4, which speeds up the breakdown of estrogen. In clinical reports, pregnancy rates jumped to over 30% when these two were taken together. And if pregnancy occurs, griseofulvin is linked to birth defects. Women taking birth control often assume it’s bulletproof. But if they’re prescribed an antifungal for athlete’s foot or ringworm, they’re being told to gamble with their fertility - and potentially their future child’s health. Pharmacists are supposed to catch this. Too often, they don’t.Warfarin: The Silent Killer in Plain Sight
Warfarin, a blood thinner, is one of the most dangerous drugs in common use - not because it’s inherently risky, but because it interacts with nearly everything. When paired with amiodarone (used for irregular heartbeat), warfarin’s levels can double or triple. Why? Amiodarone blocks the CYP2C9, CYP1A2, and CYP3A4 enzymes that break down warfarin. The result? A skyrocketing INR - meaning your blood won’t clot. A minor bump can lead to internal bleeding. A fall can be fatal. The American Academy of Family Physicians says: if you start amiodarone while on warfarin, reduce your warfarin dose by 30-50% right away. Monitor INR weekly for at least four weeks. But how many pharmacists actually do this? The data says not enough. Even statins - drugs meant to protect your heart - can make warfarin more dangerous. Fluvastatin, lovastatin, rosuvastatin, and simvastatin all inhibit CYP2C9. Atorvastatin and pravastatin? Much safer. Yet, patients are often switched without anyone checking. One wrong switch, and a patient ends up in the ER with a brain bleed.
Why Pharmacists Miss These Warnings
It’s not that pharmacists are careless. It’s that they’re drowning. In 2016, the Chicago Tribune tested 255 pharmacies. They posed as patients and asked for five known dangerous drug combinations. In over half - 52% - the pharmacist dispensed the drugs without warning. Not because they didn’t know. Because the computer system flooded them with alerts. This is called alert fatigue. A single patient might get 20-30 drug interaction warnings per prescription. Most are low-risk: “This drug might cause drowsiness.” “This combination might slightly increase blood pressure.” After seeing 100 of these a day, your brain stops listening. The real killers - the ones that cause death - get lost in the noise. A 2018 study showed that pharmacists in chain stores spend just 2.3 minutes per prescription. That’s less than 140 seconds to check a patient’s full medication list, answer questions, refill bottles, and handle insurance issues. There’s no time to dig into a complex interaction - unless the system forces them to.What’s Being Done - And What’s Still Broken
After the Tribune report, big chains like CVS and Walgreens promised change. Some did. At 12 major health systems, pharmacists implemented custom alert systems that filtered out low-risk warnings. Result? Alert volume dropped by 78%. But critical interactions - the ones that kill - were caught 89% of the time, up from 48%. That’s proof it works. But only 70% of community pharmacies have systems that can do this. The rest still blast every possible alert. And many pharmacists still don’t get training on the top 10 lethal combinations. The FDA’s 2023 Digital Health Plan is pushing AI tools that analyze your full profile - not just two drugs. Imagine a system that knows you’re 72, have kidney disease, take six meds, and just got a new antibiotic. It flags the real threats - and ignores the noise. But these tools aren’t widely used yet.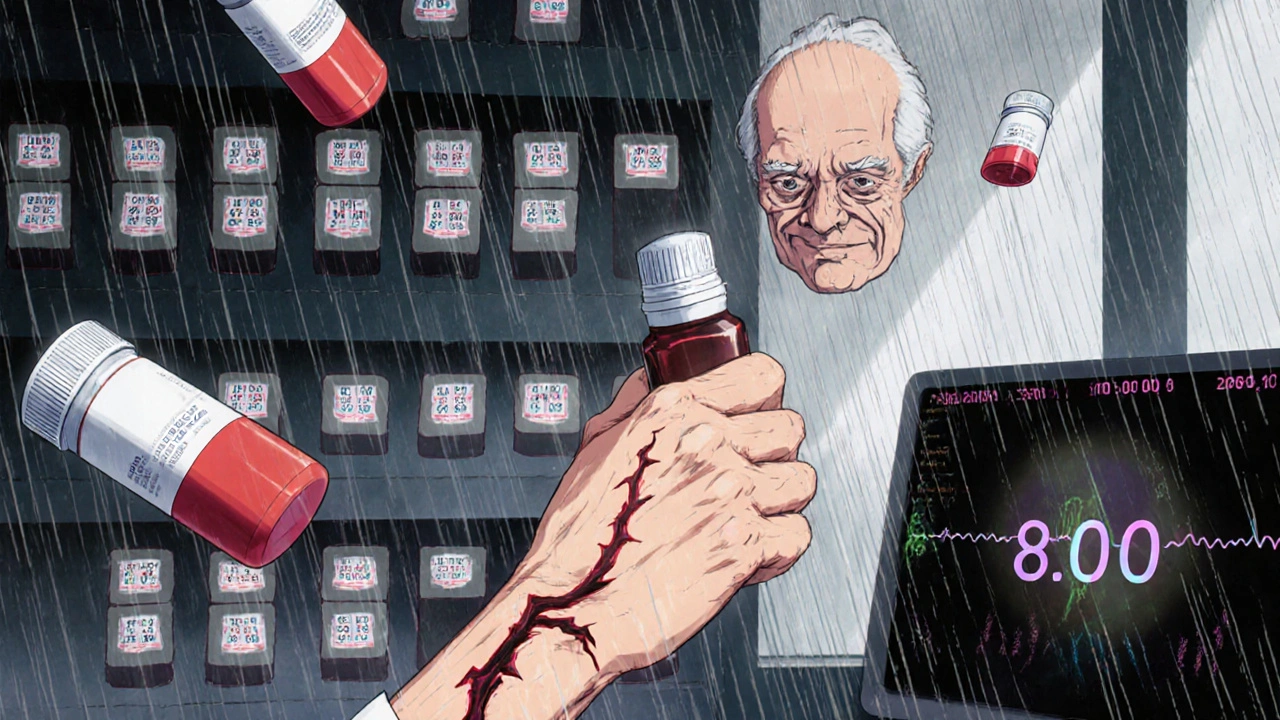
What You Can Do Right Now
You can’t wait for the system to fix itself. Here’s how to protect yourself:- Always ask: “Could this new medicine interact with anything I’m already taking?” Don’t wait for them to ask you.
- Bring your full list: Include supplements, OTC painkillers, and herbal teas. St. John’s wort can wipe out birth control. Grapefruit juice can make statins deadly.
- Know your high-risk meds: Warfarin, statins, digoxin, colchicine, benzodiazepines, opioids, and antifungals are red flags. If you’re on one, be extra careful.
- Ask for a medication review: Most pharmacies offer a free monthly review. Use it. Especially if you’ve had new prescriptions in the last 3 months.
- Don’t assume the pharmacist knows: If you’re on warfarin and get a new antibiotic, call back and ask: “Is this safe with my blood thinner?”
Who’s Most at Risk?
The data doesn’t lie. People over 65 are 7 times more likely to have a bad reaction. Why? They take an average of 4.5 prescription drugs a day. Add in OTC meds, supplements, and vitamins - and that number climbs to 8-10. That’s a recipe for disaster. Children, pregnant women, and people with liver or kidney disease are also high-risk. But most interactions are missed in older adults - because doctors and pharmacists assume “it’s just aging.” It’s not. It’s preventable.The Bottom Line
Drug interactions aren’t rare. They’re common. And deadly. The system is broken - not because pharmacists are lazy, but because they’re overloaded with noise and under-supported by technology. But you don’t have to be a victim. Your life depends on knowing which combinations to question. If you’re on warfarin and get a new antibiotic, stop. Ask. Double-check. If you’re on a statin and get a new infection, don’t just take the pill - ask if it’s safe. If you’re on birth control and get a fungal treatment - assume it won’t work until you hear otherwise. Pharmacists are on your side. But they can’t read your mind. You have to speak up.What are the most dangerous drug combinations I should watch out for?
The top lethal combinations include simvastatin + clarithromycin (risk of muscle breakdown and kidney failure), colchicine + verapamil (toxic buildup leading to organ failure), tizanidine + ciprofloxacin (sudden loss of consciousness), norgestimate/ethinyl estradiol + griseofulvin (contraceptive failure and birth defects), and warfarin + amiodarone (life-threatening bleeding). These are not theoretical - they’ve caused deaths and hospitalizations. Always check new prescriptions against your current meds.
Why don’t pharmacists always warn me about dangerous interactions?
Many pharmacies use automated systems that generate dozens of alerts per prescription - most of them low-risk. Pharmacists get so many warnings that they start ignoring them, a phenomenon called ‘alert fatigue.’ In one study, pharmacists missed over half of deadly interactions because the system flooded them with noise. Even if they know the risk, they may not have time to investigate or override the system.
Can over-the-counter drugs and supplements cause dangerous interactions?
Absolutely. St. John’s wort can reduce the effectiveness of birth control, antidepressants, and blood thinners. Grapefruit juice can make statins, blood pressure meds, and immunosuppressants dangerously strong. Even common painkillers like ibuprofen can increase bleeding risk when taken with warfarin or aspirin. Always list everything you take - including herbs, vitamins, and teas - when getting a new prescription.
What should I do if my pharmacist says a combination is safe but I’m worried?
Ask for a second opinion. Call your doctor or another pharmacy. You can also ask to speak with the pharmacist’s supervisor or request a medication review. If you’re on high-risk meds like warfarin, digoxin, or statins, never accept a quick ‘yes’ without confirmation. Your life is worth the extra 10 minutes.
Are there specific medications I should avoid if I’m over 65?
Yes. Older adults are more sensitive to drug interactions due to slower metabolism and multiple prescriptions. Avoid combining warfarin with amiodarone or certain antibiotics. Avoid statins with clarithromycin or grapefruit juice. Avoid benzodiazepines with opioids - the FDA warns this combo increases risk of fatal breathing problems. Always ask if a new drug is necessary, and if there’s a safer alternative.

Peter Aultman
November 14, 2025 AT 20:16Man I’ve had my pharmacist just shrug at me when I asked about mixing my statin with that antibiotic they gave me for a sinus infection. Thought I was overreacting until I read this. Scary how common this is. I’m just glad I didn’t end up in the ER.
Scarlett Walker
November 15, 2025 AT 02:45This is so important. My mom’s on warfarin and got prescribed a new antifungal for her toenail fungus. She didn’t think twice until I screamed at her to call the pharmacy. Turns out the pharmacist didn’t flag it either. We’re lucky she’s fine. Everyone needs to ask. Seriously.
Jane Johnson
November 15, 2025 AT 17:08While I appreciate the alarmist tone, let’s not pretend pharmacists are the only ones failing here. Doctors prescribe these combinations daily without consulting pharmacists. And patients? They don’t disclose supplements, herbs, or even grapefruit juice. The system isn’t broken-it’s being abused by negligence on every level.
Sean Evans
November 17, 2025 AT 06:58So we’re supposed to trust a system where pharmacists have 140 seconds per script? 😂 And you think the answer is just ‘ask more’? Bro. The FDA’s got AI tools that could fix this in 6 months. But nope. They’d rather keep pharmacies drowning in 30 alerts per script so they can bill for ‘medication management.’ Profit over people. Again.
Brian Bell
November 17, 2025 AT 09:59Y’all need to stop blaming pharmacists. They’re overworked AF. 😔 I work in a pharmacy and we get 50+ alerts per shift. Most are useless. When the real red flags pop up, we’re already mentally exhausted. We need better tech, not more guilt.
gent wood
November 18, 2025 AT 02:59It’s not just about the drugs-it’s about the culture of silence. Elderly patients don’t question authority. They assume the doctor knows best. The pharmacist? They’re just the person who hands over the pills. We’ve normalized this. And now people are dying because no one feels empowered to say, ‘Wait, this doesn’t feel right.’
Brittany C
November 19, 2025 AT 17:19From a clinical pharmacology standpoint, the CYP450 enzyme inhibition profiles cited are well-documented. However, the real systemic failure lies in EHR interoperability-most community pharmacies still operate on legacy systems that lack longitudinal medication reconciliation. AI-driven CDS tools with real-time polypharmacy analytics are the only scalable solution.
Anjan Patel
November 21, 2025 AT 08:04My cousin died from rhabdomyolysis after taking simvastatin and clarithromycin. The pharmacist? He said, ‘It’s fine, we’ve done it a hundred times.’ A HUNDRED TIMES?! That’s not a service-that’s a death sentence wrapped in a receipt. This isn’t negligence. It’s criminal. Someone needs to be held accountable.
Joe Goodrow
November 22, 2025 AT 12:28Why are we letting foreigners run our pharmacies? India’s got the worst drug safety standards. I bet half these pharmacists don’t even speak English properly. This is why America’s health system is crumbling. We need American-trained professionals, not cheap labor from countries where they don’t even know what CYP3A4 is.
Hrudananda Rath
November 23, 2025 AT 11:19It is truly lamentable that the sanctity of pharmaceutical care has been reduced to a transactional, algorithm-driven farce. The commodification of human health, wherein pharmacists are treated as mere clerks, is an affront to the very foundations of medical ethics. One cannot expect moral discernment from a machine-generated alert fatigue.
Nathan Hsu
November 24, 2025 AT 05:38My grandmother took warfarin, statins, and a new antibiotic-no one warned her. She had a brain bleed on a Tuesday. By Friday, she was gone. I’m not angry at the pharmacist. I’m angry that we’ve normalized this. We let corporations decide who lives and who dies based on how many alerts they can ignore. We need change. Now.
Eleanora Keene
November 25, 2025 AT 12:30You’re not alone. I used to think my pharmacist had my back-until I found out they missed the interaction between my antidepressant and my migraine med. I almost had a seizure. Now I bring a printed list, ask for a review every month, and I don’t take anything without double-checking. You’ve got power. Use it. You’re worth it.